 Blog post by Bernadette Keefe MD and Matthew Katz MD
Blog post by Bernadette Keefe MD and Matthew Katz MD
The classic ‘triple aim’ for healthcare is a framework developed by the Institute for Healthcare Improvement (IHI) that describes an approach to optimizing health system performance. IHI asserts that new designs must be developed to simultaneously pursue three dimensions which we call the ‘Triple Aim’:
- Improving the patient experience of care (including quality and satisfaction)
- Improving the health of populations, and
- Reducing the per capita cost of health care
Numerous publications suggest that the list be expanded to a ‘Quadruple Aim’ to include: Improving the Care of and Experience of The Provider (ie MDs/other HCPs). The reasoning behind this suggestion is as follows (from a BMJ editorial):
The core of workforce engagement is the experience of joy and meaning in the work of healthcare. This is not synonymous with happiness, (but) rather that all members of the workforce have a sense of accomplishment and meaning in their contributions. By meaning, we refer to the sense of importance of daily work. By joy, we refer to the feeling of success and fulfillment that results from meaningful work.
and from #95Theses by Leonard Kish and Dave Chase:
Winning healthcare delivery organizations recognize that the Quadruple Aim will deliver sustainable success. The “forgotten aim” is a better experience for the health professional. Layering more bureaucracy on top of an already-overburdened clinical team ignores that the underlying processes are frequently under-performing and that a bad professional experience negatively impacts patient outcomes.
In my opinion, this makes the utmost sense. Every parent and friend knows that without being empowered, feeling respected or validated in their own lives, they cannot help their child, their friend, or their loved one with their struggles. Our healthy feelings of wholeness, centeredness and self–esteem are intimately tied to our ability to act in an appropriately caring, and empathic manner. Without the oxygen of self-care (and the encouragement, support to do so), humans suffocate. All too often, people in the caregiving professions find it challenging to balance the needs of others and self-need.
Loss of empathy, burnout, alienation, addiction and drug abuse, depression and physician /provider suicide are all part of the sadness that happens when the needs of the provider are not given attention. It is inconceivable to me that any nation’s healthcare system would not adopt a quadruple aim approach to improve healthcare. It is my hope that through this discussion and this wonderful community’s insights that we might get closer to understanding the essential nature of mutual empathy and caring.
To this end I asked Dr Matthew Katz, @subatomicdoc, radiation oncologist at Lowell General Hospital, active healthcare social media physician and #HCLDR community member/ supporter, to join us this week. He wrote the following enlightening piece addressing the topic of care of the both the patient and physician, specifically addressing a hierarchy of needs for each. It is a pleasure to have him join me, to bring his work before the #hcldr community for discussion:
E-Patients Deserve E-Doctors: Addressing the Needs of Both to Make Healthcare Better for Everyone – (Excerpt)
By Matthew Katz, MD
Everyone deserves a chance to be healthy. Physicians, of course, focus on helping patients. Unfortunately, I often see patients’ frustrations with the health care system itself directed toward doctors.
Meanwhile, doctors are under increasing pressures on multiple fronts. Yes, we’re imperfect, but making physicians the primary focus of patient anger will not solve problems we all face as humans who will, at some point, need health care. (Note: I’m using doctors as an example for this piece, but my observations apply to all health care professionals.)
Patients need doctors. Doctors need patients. Let’s find a way to value both.
Patients deserve to be empowered
Health is more than not being ill. The World Health Organization definition puts the full range of patients’ needs first: “Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.”
How can patients achieve the health they deserve? Only if they’re empowered. The “e” in e-patient can mean many things, but if health is a basic human right, then empowerment is the only “e” ensuring that right.
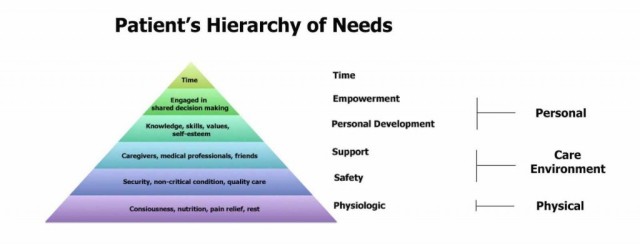
Being empowered means being able to meet certain fundamental needs, ones that need to be in place before we can make accurate, informed decisions about health. Here’s what we need for empowerment:
Image: Matthew Katz
Doctors also have a hierarchy of needs
Healers need to be healthy first—just like patients. Then, they need the right personal characteristics, training and support to be better able to do their job—helping patients.
Image: Matthew Katz
With health and virtuous characteristics as the foundation of success, doctors can earn the right to the trust of patients and their caregivers as well as society at large. This model affirms the patient-doctor relationship and aligns patients and doctors.
Making it better for everyone
We are all dissatisfied with an unhealthy health care system in a rapidly changing world. Empowering patients and doctors ensures they can work together. New technologies and tests are not solutions, they’re just tools. If patients and doctors don’t stand up for themselves, other stakeholders (e.g. hospitals, insurers, industry) may unwittingly make things worse.
Thoughtful, vocal patients, caregivers and doctors should stand together. Even when we disagree, we can respect our differences while working toward solutions, both in clinic and for the health care system.
We both have a lot to bring to the table. Empowered patients are better able to collaborate. Empowered doctors are more able to adapt to each patients needs and communicate well to build trust. We need each other. And if we support each other, the entire health care system will be the better for it.
* Please note that while physicians are used as the primary example here, truly this pertains to all healthcare providers: nursing, allied health professionals etc
Please join us on Tuesday July 21st at 8:30 PM ET (for your local time click here) using hashtag #HCLDR to discuss the following topics:
- T1 As a Patient: Does the patient hierarchy of needs answer your needs? Additional thoughts?
- T2 As an MD, does the hierarchy answer your pressing needs? Additional thoughts?
- T3 What elements of medical education produce strong yet empathetic physicians who also feel validated and empowered?
- T4 What elements in healthcare foster strong, empowered and empathetic professionals? What elements do the opposite?
Resources
The IHI Triple Aim, Institute for Healthcare Improvement, http://www.ihi.org/Engage/Initiatives/TripleAim/Pages/default.aspx accessed July 16, 2015
“From Triple Aim to Quadruple Aim: Care of the Patient Requires Care of the Provider”, Thomas Bodenheimer MD ad Christine Sinsky MD, Annals of Family Medicine, November 2014, http://www.annfammed.org/content/12/6/573.full accessed July 16 2015
“The Quadruple Aim: care, health, cost and meaning in work”, Rishi Sikka, Julianne Morath and Lucian Leape, BMJ Quality & Safety, May 16 2015, http://qualitysafety.bmj.com/content/early/2015/06/02/bmjqs-2015-004160.short?rss=1 accessed July 16 2015
“Abraham Verghese: Hope for Hands-on Medicine in the EMR Era”, John M Mandrola MD and Abraham Verghese MD, Medscap, April 6 2015, http://www.medscape.com/viewarticle/842296 (login required), accessed July 16 2015
“E-Patients Deserve E-Doctors: Addressing the Needs of Both to Make Healthcare Better for Everyone”, Matthew Katz MD, Mayo Clinic, December 29 2014, http://network.socialmedia.mayoclinic.org/discussion/e-patients-deserve-e-doctors-addressing-the-needs-of-both-to-make-healthcare-better-for-everyone-2/, accessed July 16 2015
“Slow Medicine – Not Can We Afford It, But How Can We Not”, Bernadette Keefe MD, HCLDR, November 2 2014, https://hcldr.wordpress.com/2014/11/02/slow-medicine/ accessed July 16 2015
“Why we still need human relationships in an era of digital medicine”, Liz Seegert, Association of Health Care Journalists, March 27 2015, http://healthjournalism.org/blog/2015/03/why-we-still-need-human-relationships-in-an-era-of-digital-medicine/, accessed July 16 2015
“What are the habits of highly humanistic physicians?”, Carol M Chou MD, Patient-Practitioner Relationships, Research & Humanism in Medicine, July 31 2014, http://humanism-in-medicine.org/what-are-the-habits-of-highly-humanistic-physicians/ accessed July 16 2015
“Why Are American Physicians Dying By Suicide: An Interview with Pamela Wible MD”, Chantal Oicles, ReminderCall.com Blog, June 30 2015, https://www.remindercall.com/physicians-committing-suicide/ accessed July 16 2015
“Bridging the Gap: The Doctor /Patient Relationship”, CBS News with Dr Starla Fitch, October 20 2014, https://www.youtube.com/watch?v=d7K3LKMFZOU&feature=youtu.be accessed July 16 2015
“The Darker Side of Being a Doctor”, Joanne Intile DVM, KevinMD.com, July 2 2015, http://www.kevinmd.com/blog/2015/07/the-darker-side-of-being-a-doctor.html, accessed July 16 2015
“Medicine needs to swallow a bitter pill for a healthier future”, Claire Hooker and Kimberley Ivory, The Conversation, March 13 2015, https://theconversation.com/medicine-needs-to-swallow-a-bitter-pill-for-a-healthier-future-38777, accessed July 16 2015
“Treatment ills as doctors battle depression”, Kathy Evans, The Sydney Morning Herald, September 26 2014, http://www.smh.com.au/national/treament-ills-as-doctors-battle-depression-20140925-10lupw.html, accessed July 16 2015
“Give Residents Tools To Turn Tide on Physician Burnout”, Chris Flores MD, AAFP, June 14 2015, http://blogs.aafp.org/cfr/freshperspectives/entry/give_residents_tools_to_turn, accessed July 16 2015
“Combating Physician Burnout – Lets Stop Treating Physicians Like Factory Workers”, John Lynn, EMR and EHR, July 1 2015, http://www.emrandehr.com/2015/07/01/combating-physician-burnout-lets-stop-treating-physicians-like-factory-workers/, accessed July 16 2015
“95 Theses For A New Health Ecosystem”, Dave Chase and Leonard Kish, 2015 https://medium.com/@healthrosetta/95-theses-for-a-new-health-ecosystem-b32d0cdce2ce, accessed July 16 2015
Image Credit
Angkor Table by Olivier Dolle
http://www.designersraum.com/contemporary-wood-furniture-design-of-angkor-collection-by-olivier-dolle-france/handcrafted-furniture-design-of-angkor-dining-table-by-olivier-dolle, accessed July 17, 2015

[…] Additionally both patients and physicians might appreciate this #HCLDR post. […]
[…] Additionally both patients and physicians might appreciate this post. […]
[…] used to improve the patient’s experience of their care, only then we can successfully achieve the “Quadruple aim” of healthcare: improved outcomes, better quality care, lower costs, and sustainable well-being for […]